- Lancaster School District
- Common Childhood Illnesses
Health Services/Resources
Page Navigation
-
Pink Eye
Information for staff and parents regarding pink-eye
(bacterial conjunctivitis)
Description
Pink eye is a bacterial infection of the eye resulting in redness, irritation, and discharge of fluid from the eye. It may, but not always, cause swelling of the eyelids, sensitivity to light, and discharge with mucus and pus.
In the acute phase it is typical for the eyes to be stuck together upon awaking from sleep. The absence of “sticking together in the morning” is often used as an indicator that the infection is decreasing or has passed the phase.
Transmission from one person to another
Pink-eye is transmitted from one person to another by contact with the discharge from the eye(s) or upper respiratory tract of infected individuals. It can also be transmitted by sharing eye make-up with an infected person, and by touching the hands of an infected person if they have rubbed their eyes and have the discharge from their eyes on their hands.
Treatment
It is recommended that persons suspected to have pink-eye be examined by a medical practitioner in order to have the cause of the redness diagnosed and to receive a prescription for treatment which is usually antibiotic eye-drops. Pink-eye and severe allergy resulting in redness and discharge of the eye are sometimes difficult to distinguish. If redness and discharge does not decrease after four to five days of treatment, it is important to contact the practitioner for further diagnosis.
Control of the infection
Children should not attend school during the acute phase of the infection. One way to identify that the acute phase has passed is absence of the eyes sticking together when awakening from sleep. Twenty-four hours after treatment with prescription drops has begun is commonly used as a general marker that the acute phase should have passed. However, a child should not return to school if there is still profuse discharge from the eyes. It is also important that a child returning to school understands and be able to attend to personal hygiene by avoiding rubbing of the eyes as much as possible, and by washing hands immediately if the eyes are rubbed.
Students do not need to stay home from school if a medical practitioner has determined that the cause of red and runny eyes is an allergy. When a child returns to school, following treatment for pink eye, it is a school guideline to have the child check-in through the health office to evaluate the effectiveness of treatment and to determine whether the condition is contagious.
LICE
Lice are tiny, wingless, parasitic insects that feed on your blood. Lice are easily spread — especially by schoolchildren — through close personal contact and by sharing belongings.
Signs and symptoms of lice include:
*Intense itching.
*Tickling feeling from movement of hair.
*Lice on your scalp, body, clothing, or pubic or other body hair. Adult lice may be about the size of a sesame seed or slightly larger.
*Lice eggs (nits) on hair shafts. Nits resemble tiny pussy willow buds. Nits can be mistaken for dandruff, but unlike dandruff, they can't be easily brushed out of hair.
*Small red bumps on the scalp, neck and shoulders.
Usually you can get rid of lice by taking self-care steps that include using nonprescription shampoo that's specifically formulated to kill lice.However, see your doctor if:
*Nonprescription shampoo doesn't kill the lice — your doctor can prescribe a stronger, prescription shampoo
*You're pregnant — don't use any anti-lice shampoo until you talk to your doctor
*You have any infected hives or skin abrasions from scratching
*Students may attend school while you are removing the nits, as long as there are no live lice.
*Call your School Nurse for any questions or concerns you may have.
Ringworm
Ringworm is a common skin infection that is caused by a fungus. It’s called “ringworm” because it can cause a circular rash (shaped like a ring) that is usually red and itchy. Anyone can get ringworm. The fungi that cause this infection can live on skin, surfaces, and on household items such as clothing, towels, and bedding. Treatment for ringworm usually consists of over the counter antifungal medication.
Your child may return to school as long as the affected areas have been treated for 24 hours and are drying. A Band-Aid should be applied to prevent scratching and spread of infection. The affected area must be covered either with a Band-Aid and/or clothing as long as your child is at school. Please remove the Band-Aid while your child is at home to allow air to access the site and assist with drying.
Hand-Foot-Mouth Disease
Coxsackie Virus
There has been a reported case of Hand, foot and mouth disease in your child’s classroom. Hand, foot and mouth disease is a highly contagious condition that is spread by direct contact with infected secretions from the blisters, feces, urine, and through respiratory droplets.
Symptoms include fever, runny nose, sore throat, and blister-like sores occurring on hands (palms, between fingers), soles of feet, and in the mouth (tongue, mucous membranes), and may appear 3-6 days after exposure. Although this condition is usually self-limiting, medical treatment may be required due to high fever, painful blisters (often causing loss of appetite), and secondary infection.
Children may return to school when fever and blisters are no longer present. Thorough handwashing and care with diaper changing is important. Consult your doctor or school nurse for further information.
Impetigo
What you need to know if a case of impetigo has been reported in your child’s classroom:
Impetigo is a skin infection caused by bacteria that often infects sores, insect bites, and other skin rashes. It is very contagious and can be spread easily to others.
Home Treatment for Mild Cases of Impetigo:
If your child has one or two small impetigo sores, they may be able to be treated with an over-the-counter triple antibiotic ointment or cream that you can buy without a prescription. Ask the pharmacist to help you choose one that is right for your child. Read and follow the directions on the medicine label.
Before you put the medicine on your child’s sores, remove crusty scabs by soaking all sores with warm water for 5 minutes. For sores on your child’s face, you might consider putting a warm washcloth on the area with the sores to soften the scabs. After soaking, wash the sores with warm water and an antibacterial soap. Then, use a cotton swab or your clean finger to put a small amount of the antibiotic ointment onto each of the sores. If your child has impetigo in the nose, it may be necessary to put a very small amount of ointment on a cotton swab and apply it to the sore(s) in the nose.
Wash your and your child’s hands to avoid spreading the infection to other people. Repeat the treatment three (3) times a day, or as directed on the medicine package label. Keep your child’s towel and washcloth separate from towels used by other family members. Wash washcloths, towels, bedding and clothing with hot water. Dry with high heat or in the sun.
Keep your child’s fingernails clean and cut short to keep him/her from scratching and spreading the rash. Cover the sores if they are oozing or draining. Wash your hands carefully after changing any bandages.
Your child will need to stay home from school and can return 24 hours after antibiotic treatment is started and the rash starts to heal or per physician’s orders.
When do Children with Impetigo Need to see a Healthare Provider?
Your child will need to be seen by a doctor if:
· The sores spread to another area of the body.
· There are more than just a few sores in one place.
· The sores become red, swollen, hot to touch and/or painful.
· The sores do not look like they are healing 1-2 days after medicine is started.
· Your child starts to feel sick, or
· Your child’s temperature is 101° F or higher by mouth or 100° F or higher under the arm.
For any additional questions, please feel free to call the School Nurse.
Scabies
Scabies is caused by an infestation of a mite called Sarcoptes scabiei. The scabies mite lives and lays eggs within the first layer of skin.Symptoms can take up to six weeks to make an appearance. During that time, the mites are living, multiplying, and spreading, possibly to other people.
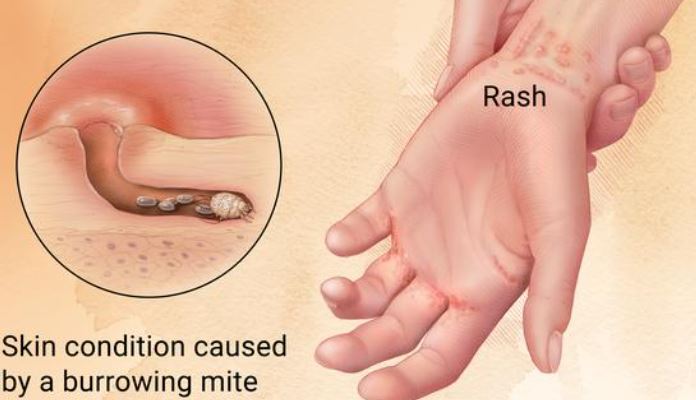
Generally, to become infected, you must be in contact — for longer than a brief moment — with a person who has scabies.Scabies can also be spread indirectly by contact with items that have been used by an infected person, which would be the case if sharing a bed or a piece of clothing, for example.The most prevalent symptom of scabies is an intensely itchy rash. The rash typically has small, pimple-like bumps within it.
Sometimes, you can see what look like tiny paths in your skin. This is where the female mites are burrowing. These paths can be skin colored or gray lines.
Scabies is sometimes confused with eczema. Eczema commonly occurs in flare-ups, meaning that sometimes it’s in full force while other times, it may not be present. Eczema typically appears in patches and may appear red with blisters on it. These blisters usually break easily and seep clear liquid. Eczema break-outs are more likely to appear on the elbows, backs of the knees, or other areas of the arms and legs. The rash may itch, and the skin may appear dry and scaly or flaky.
Treatment: Scabies must be diagnosed by a doctor and treated with prescription medication called a scabicide. If you’re diagnosed with scabies, commit to following the treatment directions completely, as reinfestation is highly possible. Please bring a doctor's note to your School Nurse.

